Second Curve of Health Care
Second Curve of Health Care
-
WHAT IS THE SECOND CURVE OF HEALTH CARE?
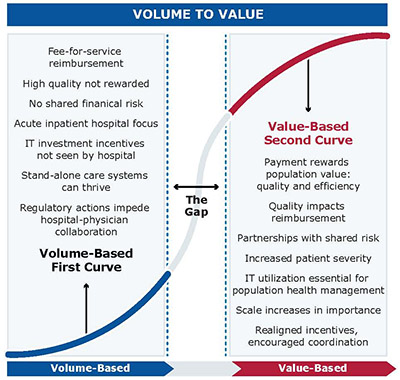
Hospitals and health systems in the United States are facing an unparalleled force to change. Industry experts have projected that multiple, intersecting pressures will drive the transformation of health care delivery and financing from volume- to value-based payments over the next decade. In the current regulatory and economic environment, hospitals must focus their efforts on performance initiatives that are essential in the short term and that will also remain critical for long-term success.
Economic futurist Ian Morrison believes that as the payment incentives shift, health care providers will go through a classic modification in their core models for business and service delivery. He refers to the volume-based environment hospitals currently face as the first curve and the future value-based market dynamic as the second curve. Progressing from the first curve to the second curve is a vital transition for hospitals.
-
Report--The Second Curve of Population Health
The Second Curve of Population Health
Though the rate and extent to which hospitals and care systems engage in population health initiatives may vary, a significant shift toward population health is anticipated in the next three to five years. The tactics described in this guide provide a framework for initiatives that hospitals and care systems could pursue to develop an institutional infrastructure that supports population health. These tactics are:
- Value-based reimbursement
- Seamless care across all settings
- Proactive and systematic patient education
- Workplace competencies and education on population health
- Integrated, comprehensive HIT that supports risk stratification of patients with real-time accessibility
- Mature community partnerships to collaborate on community-based solutions
View the accompanying Power Point presentation.
-
Infographic--The Second Curve of Population Health
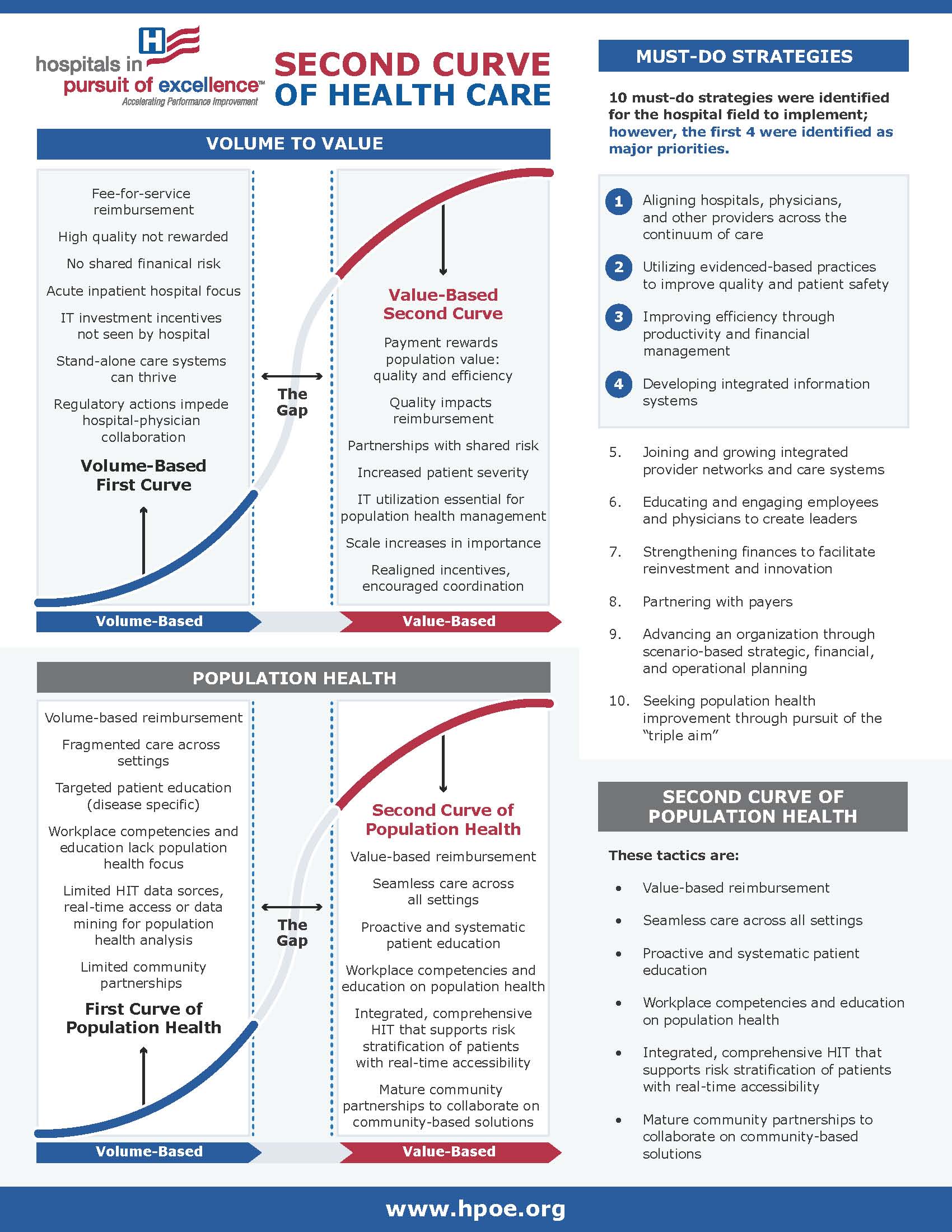
This infographic focuses on population health and life in the gap, the period between volume-based delivery and reimbursement and value-based delivery and reimbursement. It highlights the "must-do" strategies and core competencies in an easy-to-read format.
-
Report--Metrics for the Second Curve
This report provides evaluation metrics for the first four must-do strategies:
- Aligning hospitals, physicians and other clinical providers across the continuum of care
- Utilizing evidence-based practices to improve quality and patient safety
- Improving efficiency through productivity and financial management
- Developing integrated information systems
View the Power Point presentation.
-
Report--Your Hospital's Path to the Second Curve
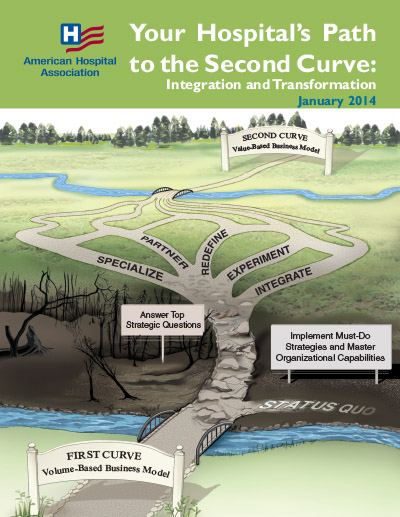
Your Hospital's Path to the Second Curve: Integration and Tranformation is the second report from the AHA Committee on Research highlighting the shift from the first curve to the value-based second curve of health care. This report outlines potentional paths to achieve the Triple Aim:
- Redefine: To a different care delivery system (i.e., either more ambulatory or oriented toward long-term care)
- Partner: With a care delivery system or health plan for greater horizontal or vertical reach, efficiency and resources for at-risk contacting (i.e., through a strategic alliance, merger or acquisition)
- Integrate: By developing a health insurance function and/or services across the continuum of care (e.g. behavioral health, home health, post-acute care, long-term care, ambulatory care)
- Experiment: With new payment and care delivery models (e.g., bundled payment, accountable care organization, medical home)
- Specialize: To become a high-performing and essential provider (e.g., children’s hospital, rehabilitation center)
View the accompanying Power Point presentation.
-
Chair Files-Webinars-Case Studies
Chair File highlighting Dignity Health: Innovative Approaches to Improve Population Health
Chair file highlighting Presbyterian Healthcare Services: Path Toward Health Care Transformation
Chair File highlighting Robert Wood Johnson Foundation initiative: Creating a Culture of Health
Infographic: Building a Leadership Team
Case study: The Progressive Journey Toward Population Health Management
-
Must-do Strategies
10 strategies were identified with the first 4 being priority.
- Align hospitals, physicians and other providers across the care continuum
- Utilize evidence-based practices to improve quality and patient safety
- Improve efficiency through productivity and financial management
- Develop integrated information systems
- Join and grow integrated provider networks and care systems
- Educate and engage employees and physicians to create leaders
- Strengthen finances to facilitate reinvestment and innovation
- Partner with payers
- Advance through scenario-based strategic, financial and operational planning
- Seek population health improvement through pursuit of the Triple Aim
-
Organizational Core Competencies
These core competencies are essential to organizations moving to value-based health care.
- Design and implementation of patient-centered, integrated care
- Creation of accountable governance and leadership
- Strategic planning in an unstable environment
- Internal and external collaboration
- Financial stewardship and enterprise risk management
- Engagement of full employee potential
- Collection and utilization of electronic data for performance improvement